1.
Nothing is more crucial to the survival and independence of organisms—be they elephants or protozoa—than the maintenance of a constant internal environment. Claude Bernard, the great French physiologist, said everything on this matter when, in the 1850s, he wrote, “La fixité du milieu intérieur est la condition de la vie libre.” Maintaining such constancy is called homeostasis. The basics of homeostasis are relatively simple but miraculously efficient at the cellular level, where ion pumps in cell membranes allow the chemical interior of cells to remain constant, whatever the vicissitudes of the external environment. More complex monitoring systems are demanded when it comes to ensuring homeostasis in multicellular organisms—animals, and human beings, in particular.
Homeostatic regulation is accomplished by the development of special nerve cells and nerve nets (plexuses) scattered throughout our bodies, as well as by direct chemical means (hormones, etc.). These scattered nerve cells and plexuses become organized into a system or confederation that is largely autonomous in its functioning; hence its name, the autonomic nervous system (ANS). The ANS was only recognized and explored in the early part of the twentieth century, whereas many of the functions of the central nervous system (CNS), especially the brain, had already been mapped in detail in the nineteenth century. This is something of a paradox, for the autonomic nervous system evolved long before the central nervous system.
They were (and to a considerable extent still are) independent evolutions, extremely different in organization, as well as formation. Central nervous systems, along with muscles and sense organs, evolved to allow animals to get around in the world—forage, hunt, seek mates, avoid or fight enemies, etc. The central nervous system, with its sense organs (including those in the joints, the muscles, the movable parts of the body), tells one who one is and what one is doing. The autonomic nervous system, sleeplessly monitoring every organ and tissue in the body, tells one how one is. Curiously, the brain itself has no sense organs, which is why one can have gross disorders here, yet feel no malaise. Thus Ralph Waldo Emerson, who developed Alzheimer’s disease in his sixties, would say, “I have lost my mental faculties but am perfectly well.”
By the early twentieth century, two general divisions of the autonomic nervous system were recognized: a “sympathetic” part, which, by increasing the heart’s output, sharpening the senses, and tensing the muscles, readies an animal for action (in extreme situations, for instance, life-saving fight or flight); and the corresponding opposite—a “parasympathetic” part—which increases activity in the “housekeeping” parts of the body (gut, kidneys, liver, etc.), slowing the heart and promoting relaxation and sleep. These two portions of the ANS work, normally, in a happy reciprocity; thus the delicious postprandial somnolence that follows a heavy meal is not the time to run a race or get into a fight. When the two parts of the ANS are working harmoniously together, one feels “well,” or “normal.”
No one has written more eloquently about this than Antonio Damasio in his book The Feeling of What Happens and many subsequent books and papers. He speaks of a “core consciousness,” the basic feeling of how one is, which eventually becomes a dim, implicit feeling of consciousness.1 It is especially when things are going wrong, internally—when homeostasis is not being maintained; when the autonomic balance starts listing heavily to one side or the other—that this core consciousness, the feeling of how one is, takes on an intrusive, unpleasant quality, and now one will say, “I feel ill—something is amiss.” At such times one no longer looks well either.
As an example of this, migraine is a sort of prototype illness, often very unpleasant but transient, and self-limiting; benign in the sense that it does not cause death or serious injury and that it is not associated with any tissue damage or trauma or infection; and occurring only as an often-hereditary disturbance of the nervous system. Migraine provides, in miniature, the essential features of being ill—of trouble inside the body—without actual illness.
When I came to New York, nearly fifty years ago, the first patients I saw suffered from attacks of migraine—“common migraine,” so called because it attacks at least 10 percent of the population. (I myself have had attacks of them throughout my life.2) Seeing such patients, trying to understand or help them, constituted my apprenticeship in medicine—and led to my first book, Migraine.
Though there are many (one is tempted to say, innumerable) possible presentations of common migraine—I described nearly a hundred such in my book—its commonest harbinger may be just an indefinable but undeniable feeling of something amiss. This is exactly what Emil du Bois-Reymond emphasized when, in 1860, he described his own attacks of migraine: “I wake,” he writes, “with a general feeling of disorder….”
Advertisement
In his case (he had had migraines every three to four weeks, since his twentieth year), there would be “a slight pain in the region of the right temple which…reaches its greatest intensity at midday; towards evening it usually passes off…. At rest the pain is bearable, but it is increased by motion to a high degree of violence…. It responds to each beat of the temporal artery.” Moreover, du Bois-Reymond looked different during his migraines: “The countenance is pale and sunken, the right eye small and reddened.” During violent attacks he would experience nausea and “gastric disorder.” The “general feeling of disorder” that so often inaugurates migraines may continue, getting more and more severe in the course of an attack; the worst- affected patients may be reduced to lying in a leaden haze, feeling half-dead, or even that death would be preferable.3
I cite du Bois-Reymond’s self- description, as I do at the very beginning of Migraine, partly for its precision and beauty (as are common in nineteenth-century neurological descriptions, but rare now), but above all, because it is exemplary—all cases of migraine vary, but they are, so to speak, permutations of his.
The vascular and visceral symptoms of migraine are typical of unbridled parasympathetic activity, but they may be preceded by a physiologically opposite state. One may feel full of energy, even a sort of euphoria, for a few hours before a migraine—George Eliot would speak of herself as feeling “dangerously well” at such times. There may, similarly, especially if the suffering has been very intense, be a “rebound” after a migraine. This was very clear with one of my patients (Case #68 in Migraine), a young mathematician with very severe migraines. For him the resolution of a migraine, accompanied by a huge passage of pale urine, was always followed by a burst of original mathematical thinking. “Curing” his migraines, we found, “cured” his mathematical creativity, and he elected, given this strange economy of body and mind, to keep both.
While this is the general pattern of a migraine, there can occur rapidly changing fluctuations and contradictory symptoms—a feeling that patients often call “unsettled.” In this unsettled state (I wrote in Migraine), “one may feel hot or cold, or both…bloated and tight, or loose and queasy; a peculiar tension, or languor, or both…sundry strains and discomforts, which come and go.”
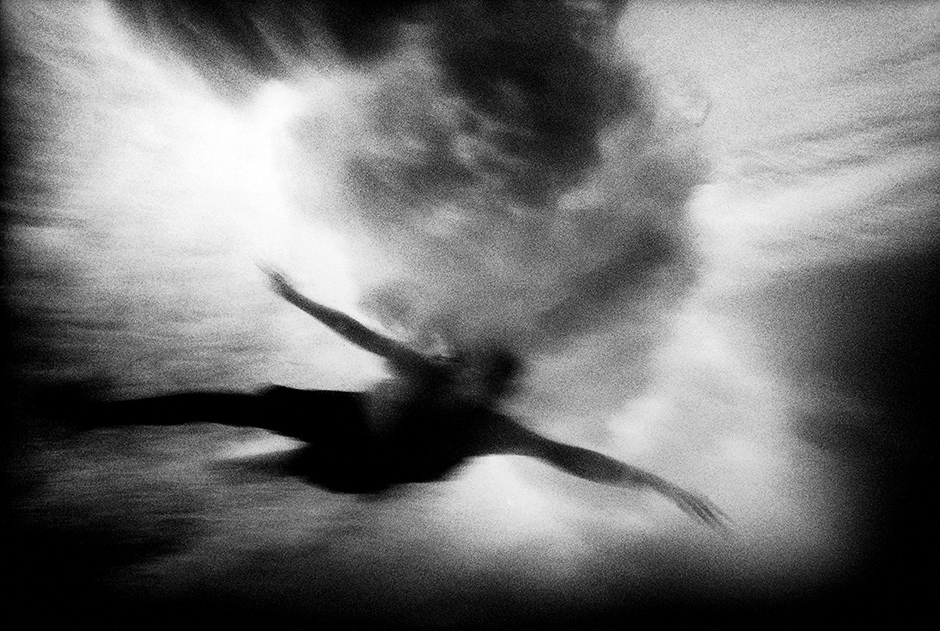
Indeed, everything comes and goes, and if one could take a scan or inner photograph of the body at such times, one would see vascular beds opening and closing, peristalsis accelerating or stopping, viscera squirming or tightening in spasms, secretions suddenly increasing or decreasing—as if the nervous system itself were in a state of indecision. Instability, fluctuation, and oscillation are of the essence in the unsettled state, this general feeling of disorder. We lose the normal feeling of “wellness,” which all of us, and perhaps all animals, have in health.
2.
If new thoughts about illness and recovery—or old thoughts in new form—have been stimulated by thinking back to my first patients, they have been given an unexpected salience by a very different personal experience in recent weeks.
On Monday, February 16, I could say I felt well, in my usual state of health—at least such health and energy as a fairly active eighty-one-year-old can hope to enjoy—and this despite learning, a month earlier, that much of my liver was occupied by metastatic cancer. Various palliative treatments had been suggested—treatments that might reduce the load of metastases in my liver and permit a few extra months of life. The one I opted for, decided to try first, involved my surgeon, an interventional radiologist, threading a catheter up to the bifurcation of the hepatic artery, and then injecting a mass of tiny beads into the right hepatic artery, where they would be carried to the smallest arterioles, blocking these, cutting off the blood supply and oxygen needed by the metastases—in effect, starving and asphyxiating them to death. (My surgeon, who has a gift for vivid metaphor, compared this to killing rats in the basement; or, in a pleasanter image, mowing down the dandelions on the back lawn.) If such an embolization proved to be effective, and tolerated, it could be done on the other side of the liver (the dandelions on the front lawn) a month or so later.
The procedure, though relatively benign, would lead to the death of a huge mass of melanoma cells (almost 50 percent of my liver had been occupied by metastases). These, in dying, would give off a variety of unpleasant and pain-producing substances, and would then have to be removed, as all dead material must be removed from the body. This immense task of garbage disposal would be undertaken by cells of the immune system—macrophages—that are specialized to engulf alien or dead matter in the body. I might think of them, my surgeon suggested, as tiny spiders, millions or perhaps billions in number, scurrying inside me, engulfing the melanoma debris. This enormous cellular task would sap all my energy, and I would feel, in consequence, a tiredness beyond anything I had ever felt before, to say nothing of pain and other problems.
Advertisement
I am glad I was forewarned, for the following day (Tuesday, the seventeenth), soon after waking from the embolization—it was performed under general anesthesia—I was to be assailed by feelings of excruciating tiredness and paroxysms of sleep so abrupt they could poleaxe me in the middle of a sentence or a mouthful, or when visiting friends were talking or laughing loudly a yard away from me. Sometimes, too, delirium would seize me within seconds, even in the middle of handwriting. I felt extremely weak and inert—I would sometimes sit motionless until hoisted to my feet and walked by two helpers. While pain seemed tolerable at rest, an involuntary movement such as a sneeze or hiccup would produce an explosion, a sort of negative orgasm of pain, despite my being maintained, like all post-embolization patients, on a continuous intravenous infusion of narcotics. This massive infusion of narcotics halted all bowel activity for nearly a week, so that everything I ate—I had no appetite, but had to “take nourishment,” as the nursing staff put it—was retained inside me.
Another problem—not uncommon after the embolization of a large part of the liver—was a release of ADH, anti-diuretic hormone, which caused an enormous accumulation of fluid in my body. My feet became so swollen they were almost unrecognizable as feet, and I developed a thick tire of edema around my trunk. This “hyperhydration” led to lowered levels of sodium in my blood, which probably contributed to my deliria. With all this, and a variety of other symptoms—temperature regulation was unstable, I would be hot one minute, cold the next—I felt awful. I had “a general feeling of disorder” raised to an almost infinite degree. If I had to feel like this from now on, I kept thinking, I would sooner be dead.
I stayed in the hospital for six days after embolization, and then returned home. Although I still felt worse than I had ever felt in my life, I did in fact feel a little better, minimally better, with each passing day (and everyone told me, as they tend to tell sick people, that I was looking “great”). I still had sudden, overwhelming paroxysms of sleep, but I forced myself to work, correcting the galleys of my autobiography (even though I might fall asleep in mid-sentence, my head dropping heavily onto the galleys, my hand still clutching a pen). These post-embolization days would have been very difficult to endure without this task (which was also a joy).
On day ten, I turned a corner—I felt awful, as usual, in the morning, but a completely different person in the afternoon. This was delightful, and wholly unexpected: there was no intimation, beforehand, that such a transformation was about to happen. I regained some appetite, my bowels started working again, and on February 28 and March 1, I had a huge and delicious diuresis, losing fifteen pounds over the course of two days. I suddenly found myself full of physical and creative energy and a euphoria almost akin to hypomania. I strode up and down the corridor in my apartment building while exuberant thoughts rushed through my mind.
How much of this was a reestablishment of balance in the body; how much an autonomic rebound after a profound autonomic depression; how much other physiological factors; and how much the sheer joy of writing, I do not know. But my transformed state and feeling were, I suspect, very close to what Nietzsche experienced after a period of illness and expressed so lyrically in The Gay Science:
Gratitude pours forth continually, as if the unexpected had just happened—the gratitude of a convalescent—for convalescence was unexpected…. The rejoicing of strength that is returning, of a reawakened faith in a tomorrow and the day after tomorrow, of a sudden sense and anticipation of a future, of impending adventures, of seas that are open again.
Epilogue
The hepatic artery embolization destroyed 80 percent of the tumors in my liver. Now, three weeks later, I am having the remainder of the metastases embolized. With this, I hope I may feel really well for three or four months, in a way that, perhaps, with so many metastases growing inside me and draining my energy for a year or more, would scarcely have been possible before.
This Issue
April 23, 2015
Monsters Together
‘A New Way of Writing About Race’
-
1
Antonio Damasio and Gil B. Carvalho, “The Nature of Feelings: Evolutionary and Neurobiological Origins,” Nature Reviews Neuroscience, Vol. 14 (February 2013). ↩
-
2
I also have attacks of “migraine aura,” with scintillating zigzag patterns and other visual phenomena. They, for me, have no obvious relation to my “common” migraines, but for many others the two are linked, this hybrid attack being called a “classical” migraine. ↩
-
3
Aretaeus noted in the second century that patients in such a state “are weary of life and wish to die.” Such feelings, while they may originate, and be correlated with, autonomic imbalance, must connect with those “central” parts of the ANS in which feeling, mood, sentience, and (core) consciousness are mediated—the brainstem, hypothalamus, amygdala, and other subcortical structures. ↩