1.
During the nineteenth century, Britain was struck by four epidemics of cholera, an often fatal disease characterized by attacks of diarrhea so intense that the body may lose gallons of water in just a few hours. The horrifying symptoms—dehydration so severe that the flesh shrinks back against the skull and the blood turns to jelly—appeared suddenly, and death could follow in the same day. It felt “like being hit with a club,” reported one survivor.1
Doctors, desperate to conceal their powerlessness, prescribed the following as “cures”: boiling water applied to the belly, electric shocks, enemas of turpentine and mutton stew, and gunpowder fired into the air in the vicinity of the patient. The public variously attributed the disease to ozone, ionic fields and other disturbances of the atmosphere, fumes produced by rotting sewage and putrescent yeast, and poison administered by doctors: at the time there was strong demand in medical schools for cadavers for dissection purposes, and this led to a spate of much-publicized murders, some of which were rumored to be linked to the cholera epidemics.2
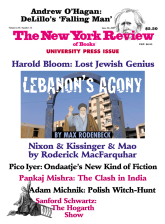
Steven Johnson’s The Ghost Map tells the story of how the mystery of cholera transmission was solved by an ingenious physician named John Snow and how his discovery helped eliminate cholera from Britain and eventually from the Western world. But it also tells a parallel story about how a modern state bureaucracy emerged to confront one of the many novel challenges posed by urbanization. Nineteenth-century London was characterized by great civic turmoil. Never before had three million people lived together in so limited a space, and as Johnson points out, some doubted whether such a dense settlement was sustainable at all. Writer and publisher Sir Richard Phillips, whom Johnson quotes, even suggested there was something dangerous in the idea of the city itself:
The houses will become too numerous for the inhabitants, and certain districts will be occupied by beggary and vice or become depopulated. The disease will spread like an atrophy in the human body, and ruin will follow ruin, till the entire city is disgusting to the remnant of the inhabitants…. Such have been the causes of decay of all overgrown cities. Nineveh, Babylon, Antioch, and Thebes are become heaps of ruins….
The growth of cities and towns set off by the industrial revolution would forever transform the economy and culture of the West, but it also caused unprecedented upheavals, including vast inequalities in wealth, class tensions, the weakening of social ties, and overcrowding and squalor of an order previously unknown. These last conditions provided new niches for deadly diseases like cholera that could not spread through scattered rural populations.
Public coordination was required to manage a sprawling urban organism like London, and various government offices emerged to oversee the paving and lighting of streets, the collection of taxes, the construction and management of sewers, drains, prisons, and workhouses, and to respond to crises such as epidemics. Like the compartments of some giant developing brain, these offices were both crucial to the functioning of the creature of which they were a part, and also prone to mistakes.
One of the greatest challenges to urban life in the nineteenth century was the question of what to do with what Johnson calls the “rising tide of excrement” piling up under the feet of the population of London and other cities. At the time the custom was to throw one’s waste out the back window or store it in overflowing cesspools and cellars. An 1849 survey found that in London, one home in five stank of human waste, and one in twenty contained heaps of shit in the cellar. “At mid-century Victorian England was in danger of becoming submerged in a huge dung-heap of its own making,” wrote historian Anthony Wohl.3
The situation was alarming not only for the obvious reasons but also because the prevailing theory at the time held that diseases were caused not by germs but by “miasmas”—the bad smells emitted by sewage and rotting animal and vegetable matter. This idea, derived from ancient Greece, was seldom questioned. After all, the effect of disgusting smells on the appetite and digestion was well known, especially in the nineteenth century. “If we were to be transported back to a nineteenth-century town,” Wohl tells us, “it is probable that…we would be able to proceed only at risk of heaving stomach and nausea.” Thus when cholera, an ancient disease, spread west from its original breeding ground in South Asia during the 1820s and 1830s, it was immediately attributed to the clouds of miasma forming over Europe’s growing cities.
In 1842, the British social reformer Edwin Chadwick issued a report showing that the health of people living in towns was much worse than that of rural dwellers, and for the next twelve years, he dedicated himself to solving the problem of urban miasma. As head of the newly created General Board of Health, he launched a crusade to force reluctant taxpayers to fund the construction of an expanded sewer system that would clean out the cesspools and cellars of London. His efforts resulted in some progress, but unfortunately, the sewers he commissioned emptied right into the Thames River, which over the preceding decades had been “transformed from a fishing ground teeming with salmon to one of the most polluted waterways in the world,” even as much of the city’s drinking water continued to be drawn from it.
Advertisement
Since cholera germs normally spread by what epidemiologists call the “fecal-oral route,” Chadwick had thus inadvertently turned a pathway for their transmission into a superhighway. Some historians have deemphasized or even overlooked entirely the disastrous effects of this policy, arguing instead that Chadwick did the right thing (build sewers) for the wrong reason (to prevent disease by getting rid of smelly miasmas). Johnson emphasizes Chadwick’s mistake and shows that, as usual, bad science led to bad policy. It is likely that the severity of the cholera epidemics of 1848–1849 and 1854, which killed tens of thousands of people, was partly attributable to Chadwick’s sewers.
At around this time John Snow, an austere but ingenious London physician from a humble background in the north of England, produced a thirty-one-page monograph that explained cholera outbreaks once and for all. Or it would have, if it had been taken more seriously. Snow had encountered cholera during Britain’s first epidemic of 1831–1832, when he was working as an apothecary’s apprentice in Newcastle. He was struck by the pitiful squalor in which the victims lived, but he must have noticed that the disease didn’t always strike those who were most exposed to “miasmas.” For example, many of the “night soil men,” whose work brought them into very close contact with the most repulsive fumes, were spared.
The idea that cholera was transmitted through contaminated water had been suggested in medical circles from time to time, and when cholera struck again in 1848–1849, Snow observed that the only characteristic the victims seemed to share was access to a particular water source. It would be more than thirty years before Robert Koch identified the cholera bacterium under a microscope, and Snow’s insight, well described by Johnson, testifies to the power of the scientific imagination at its most creative.
Snow published his findings in the London Medical Gazette in 1849, but the medical community by and large dismissed them. It is not clear why, but many doctors, having devoted their careers to peddling the “cures” I have mentioned—mutton enemas and so on—based on the “miasma” theory might have been slow to entertain alternative ideas. Consciously or not, civic leaders may have been biased against the water-borne theory because of the huge expense involved in the implied remedy: a reliable system of sewers and pumps to remove human waste from the water supply. Moreover, Snow was an outsider; he hadn’t gone to Oxford or Cambridge and was awkward and shy when presenting his views in public. His findings relied on the techniques of the fledgling science of epidemiology—the measurement of disease in the messy real world rather than the controlled environment of a lab. Whatever the reason, the London Medical Gazette suggested one way in which Snow’s theory would stand or fall:
The experimentum crucis would be, that the water conveyed to a distant locality, where cholera had been hitherto unknown, produced the disease in all who used it, while those who did not use it, escaped.
This “crucial experiment” was soon made possible by the cholera epidemic of 1854. The outbreak struck South London first. When Snow went to investigate, he found that not every house was affected. By going door to door interviewing people, he was able to show that the stricken houses obtained water from a company that drew its supply directly from the filthiest part of the Thames. Those households that were spared obtained water from another company that drew from cleaner sources upstream. Snow then rushed to Soho, where another explosive outbreak was underway. There, he found that shortly before becoming ill, virtually every cholera victim had drunk water from the same pump, located on Broad Street. Very few people who did not drink Broad Street pump-water fell ill. Snow obtained permission from the Board of Health to remove the handle of the Broad Street pump, which, Johnson argues, may well have prevented another outbreak and saved many lives.
Months after the epidemic had passed, Snow drew a map showing the locations of the victims of the Soho outbreak. Today this map is one of the most famous documents in the history of science, but it made little impression at the time. Instead, the Board of Health produced a report of over one hundred pages focusing almost entirely on the quality of the air in London during the outbreak—wind speeds, ozone, and so on. Regarding Snow’s theory, the authors maintained, “We see no reason to adopt this belief.” When Snow died in 1858, his thirty-three-word obituary in The Lancet, which also had yet to embrace the germ theory, did not mention his contributions to the study of cholera at all.
Advertisement
But during the very summer of Snow’s death, opinion was beginning to turn in his direction. It was a particularly steamy and hot season and by June the Thames had become a putrescent stew. As its noxious contents floated past Parliament, the stench finally persuaded MPs that it was time—whatever the expense—to commission a vast system of sewers and pumps to transport London’s excrement far out of town. The completion of this system in 1867 was an occasion for national rejoicing and one sewage pumping station was even opened by the Prince of Wales. By now, news of Pasteur’s experiments with fermentation and the growing recognition that the miasma theory could not explain many of the facts about cholera had brought members of the medical community around to Snow’s point of view. Cholera would soon become a distant nightmare outside of the developing world.
The story of Britain’s cholera epidemics is partly about how one inspired genius perceived the truth through the miasma of vested interests, prejudice, and entrenched opinion. But it is also about the power of measurement. Snow’s investigations would never have been possible without the reports produced by England’s General Registry Office, the successor institution of a system of parish registers that had been tracking births and deaths throughout England since the mid-seventeenth century. Across Western Europe, this was a time of increasing concern with statistical precision. Census bureaus and other offices were being set up to count populations, calculate land holdings for tax purposes, weigh and measure army recruits, calculate crime rates, and otherwise numerically characterize populations.4
During the 1850s, the General Registry Office was headed by William Farr, whose surveillance of the cholera epidemic was a masterpiece of nineteenth-century population measurement. His daily records noted not only when the cases occurred, but where the victims lived, and they were publicly available to all. In those days, the GRO was something of an activist organization. Farr, like Chadwick, believed that market forces alone would never solve all of society’s problems, and in order to shame local governments into action he publicly identified the districts in England with the highest death rates. It worked: in 1846, he showed that half of all children in Liverpool died by age six; that year, the Liverpool government rushed to pass new hygiene legislation two years before Parliament passed similar legislation for the entire nation.5
2.
Because statistics tend to deal in averages, medians, and other collective measures, they cannot capture the particular experiences of those—the poor, the creative, the eccentric, for example—whose experience is far from the mean. Charles Dickens’s Hard Times, published in 1854, during the heyday of Utilitarianism and the growth of England’s civic bureaucracies, contained an implicit attack on the abuse of statistical knowledge. Thomas Gradgrind, the fact-obsessed schoolmaster at the center of the story, saw every human experience in terms of general probabilities, and could not fathom emotion, art, or feeling.6 Similarly, in the twentieth century Michel Foucault saw statistical surveys as instruments of a “Panopticon”-like state bent on controlling the minds and bodies of its citizens. Certainly the keeping of statistics has sometimes enabled a kind of routinized process of depersonalization that distances people from their essential humanity. The death lists kept by Nazi bureaucrats apparently obscured for many of them the reality of what they were involved in.
But such abuses are not intrinsic to statistical surveillance. After all, as the Cambridge historian Simon Szreter points out, just because the Jews were transported to Auschwitz on trains does not mean that railroads are intrinsically evil. Szreter reminds us that registration of one’s birth and death is enshrined in the Universal Declaration of Human Rights, and as a precondition for security of property and citizenship, it is probably essential for economic development and democracy as well.7
Johnson ends The Ghost Map with an apocalyptic warning about the threats new germs such as bird flu still pose to human health. This is the only part of the book about which I found myself skeptical. Researchers now suspect that the mutations required to transform the bird flu virus into one that spreads easily among humans are unlikely to occur.8 Even if they do, we have two weapons that the British didn’t have in the days of cholera. First we understand the germ theory, so we know where the threat is coming from and how to fight it with drugs, vaccines, and changes in behavior. Second, we have an extensive global surveillance system that alerts us to new outbreaks of disease so we can respond to them before they have spread widely.
This system for reporting and response isn’t perfect, but where it is in place it works pretty well. Surveys alone cannot protect human health, but they are essential because the numbers tell us what to do. Florence Nightingale even maintained that statistics were instructions from God that we ignore at our peril.
What would it be like to live in a world without numbers? I got a sense of this on a recent trip to East Africa, where the failure to register births and deaths and monitor diseases is responsible for thousands of deaths each year. I was visiting a program called the Tanzania Essential Health Interventions Project, or TEHIP, which was established in two of Tanzania’s 127 districts in 1997. By 2002, the death rate of children in both districts had been cut dramatically but it had remained stable and high elsewhere in the country. In 2005, the Tanzanian government began to implement the program throughout the country, and by 2007, the national child mortality rate, which had barely improved at all between 1990 and 2000, had fallen by 25 percent. Elsewhere in East Africa, no such decline has occurred. TEHIP’s budget is tiny by foreign aid standards—the districts spent on average about $1 per resident on the program, an amazing bargain compared to other health initiatives funded by donors such as the US government, the World Bank, and the Gates Foundation.9
What was the secret of TEHIP’s success? Record-keeping and statistics. The first thing you see when you walk into a TEHIP clinic is a wall chart, drawn in magic marker on butcher paper, showing graphs and tables indicating the case rates of different diseases. From this, health workers can tell which drugs they will need the following month. They also keep detailed ledgers of spending on salaries and procurement of supplies and spare parts for vehicles and radios, staff absences, and so on. Inspectors from the district headquarters visit each clinic from time to time, to ensure that records are being kept properly.
Before TEHIP, it sometimes seemed as though chaos reigned. Medicines were supplied in pre-packaged kits shipped from Europe, but their contents had been decided on in the early 1980s, and since then, the epidemiological situation had changed considerably. The population had grown and rates of malaria had increased in the lowlands, while rates of pneumonia had risen in the highlands. Thus the drugs to treat these conditions often ran out before the next kit arrived. Bizarre mistakes sometimes occurred: “Once we opened the kit and it was full of epilepsy drugs, but there are no cases of epilepsy around here,” one doctor told me. Medical staff members complained, but because the consequences of this epidemiological shift were not being measured, nothing changed.
The arrival of salaries was desultory, so some doctors and nurses, unpaid for months, sought other livelihoods. The system for procuring spare parts functioned poorly, so radios and vehicles often broke down, making communication with the health care system all but impossible. Measles and cholera killed hundreds of people because reporting an outbreak often involved a long trek by foot through the bush to a main road followed by a public bus ride to a faraway town where the district health authorities were located. Help might take days to arrive. Now epidemics can be reported instantly because the supply chain for spare parts functions; since the program started, there have been virtually no deaths from measles or cholera in the TEHIP districts.10
By far, the worst health problem in Tanzania is malaria. Within days of being bitten by a malaria-carrying mosquito, the victim’s blood teems with parasites that cause anemia, headaches, vomiting, and swings of intense fevers and chills. The disease kills roughly a million people in Africa each year, most of them children. In some cases, the parasites spread to the brain, causing the entire body to seize up and shake rigidly as if possessed by an alien spirit. The eyes roll backward so only the whites are showing, and the mouth fills with froth. If the victim survives, he may be brain-damaged for life.
Malaria is curable. A range of drugs can kill the parasites, bring down the fevers, and calm the convulsions; but in this region, local people often mistake the symptoms for degedege—an evil bird that supposedly flies over children trying to get inside them. In a mirror image of the “miasma” theory, this bird is believed to hate bad smells, so traditional healers in Tanzania sell poor women elephant dung which they burn in the hope that the fumes will chase the bird away.
In 1997, Charles Mayombana, a medical researcher from the Tanzanian Health Ministry, was studying this and other local beliefs when he made a troubling discovery. Some 80 percent of the mothers of children who died of malaria in one district had actually sought help from a government health clinic or pharmacy for treatment as soon as they noticed the early symptoms of the disease—the fevers, chills, vomiting, and headaches. However, the treatment they received was so bad that the disease, rather than being cured, progressed to the seizure stage.11
At some clinics, days and even weeks would go by with no doctor or nurse in attendance. At others, there was no medicine, or if there was, chances are it was a drug called chloroquine, which is ineffective in Tanzania because a large fraction of malaria parasites are resistant to it. As their children’s symptoms worsened, the mothers watched in desperation, and they wondered if the doctors had been wrong. Perhaps this was not malaria after all. Perhaps it was witchcraft, or some other “African” disease that Western medicine can’t cure. So, like the panicked residents of nineteenth-century London, they turned to quacks for help. But since TEHIP started, deaths from malaria have fallen steeply, and the belief that it can be cured by elephant dung is dying out.
Reporting births, deaths, and cases of disease, tracking drugs and supplies, managing salaries and contracts, maintaining ledgers, and creating a system of inspections may not sound like the stuff of great medical heroics, but they are. There can even be drama in developing surveillance systems. Last year, when technicians from the Tanzanian Health Ministry were upgrading the ministry’s health accounts software—the spreadsheets used to track procurement and spending—“there was this electricity in the air,” says Don de Savigny, a public health researcher who has worked in Tanzania for twenty years. “They had an energy I have never seen before. The programmers were up all night and there were sparks going off in the hotel room.”
A growing number of donors and philanthropists, including the Gates Foundation and the World Bank, are now funding programs to improve disease surveillance in Africa,12 and The Lancet recently published a series of articles on the subject.13 Some officials in the Tanzanian Ministry of Health have been urging the government to create a village-based system for registering births and deaths for the entire country. This would allow them to do what William Farr did: identify the unhealthiest districts and shame local governments into action. But according to one ministry official, some parliamentarians resist the idea. “These politicians,” he lamented to me, “some of them just don’t want to know.”
This Issue
June 28, 2007
-
1
Sandra Hempel, The Medical Detective: John Snow and the Mystery of Cholera (Granta, 2006), p. 3.
↩ -
2
Hempel, The Medical Detective, pp. 36, 46–47, 52, 56, 78.
↩ -
3
Anthony S. Wohl, Endangered Lives: Public Health in Victorian Britain (Harvard University Press, 1983), p. 86.
↩ -
4
See I. Bernard Cohen, The Triumph of Numbers: How Counting Shaped Modern Life (Norton, 2005).
↩ -
5
See Simon Szreter, “The G.R.O. and the Public Health Movement in Britain, 1837–1914,” in Health and Wealth: Studies in History and Policy (University of Rochester Press, 2005).
↩ -
6
See Cohen, The Triumph of Numbers, for further discussion of Dickens’s attitude toward statistics.
↩ -
7
Simon Szreter, “The Right of Registration: Development, Identity Registration, and Social Security—A Historical Perspective,” World Development, Vol. 35, No. 1 (2007), pp. 67–86.
↩ -
8
See Nicholas Wade, “Studies Suggest Pandemic Isn’t Imminent,” The New York Times, March 23, 2006.
↩ -
9
Interested readers can find out more about the TEHIP program from the Web site of the International Development Research Center: www.idrc.ca/en/ev-3170-201-1-DO_TOPIC.html. See also Don de Savigny, Harun Kasale, Conrad Mbuya, and Graham Reid, Fixing Health Systems (Ottawa: International Development Research Centre, 2004).
↩ -
10
Tanzania Ministry of Health and Social Welfare, “District Health Services Profile—2005 Rural Coastal Districts: Rufiji DSS Sentinel District Information for Districts of Lindi, Mtwara, Pwani and Tanga Regions” (Dar-es-Salaam, 2006).
↩ -
11
Charles Chrisostom Mayombana, Local Understanding and Practices Related to IMCI Interventions in Eastern Tanzania, Ph.D. dissertation, University of Basel, Switzerland (2004); see also Don de Savigny et al., “Care-Seeking Patterns for Fatal Malaria in Tanzania,” Malaria Journal, Vol. 3, No. 27 (July 28, 2004).
↩ -
12
See, for example, the Web site of the INDEPTH Network, a clearing house for health surveillance in Africa: www.indepth-network.org.
↩ -
13
J. Ties Boerma and Sally K. Stansfield, “Health Statistics Now: Are We Making the Right Investments?” The Lancet, Vol. 369 (March 3, 2007), pp. 779–786; Ties Boerma and Carla Abou-Zahr “Health Statistics Are No Longer Boring!” The Lancet, Vol. 369 (March 3, 2007), pp. 718–719; Neff Walker, Jennifer Bryce, and Robert E. Black, “Interpreting Health Statistics for Policymaking: The Story Behind the Headlines,” The Lancet, Vol. 369 (March 3, 2007), pp. 956–963.
↩