In his valedictory State of the Union address this January, President Obama endorsed Vice President Biden’s proposal of last October that the US needed something like a “moonshot” to cure cancer. “Tonight, I’m announcing a new national effort to get it done,” Obama said. “For the loved ones we’ve all lost, for the families that we can still save, let’s make America the country that cures cancer once and for all.”
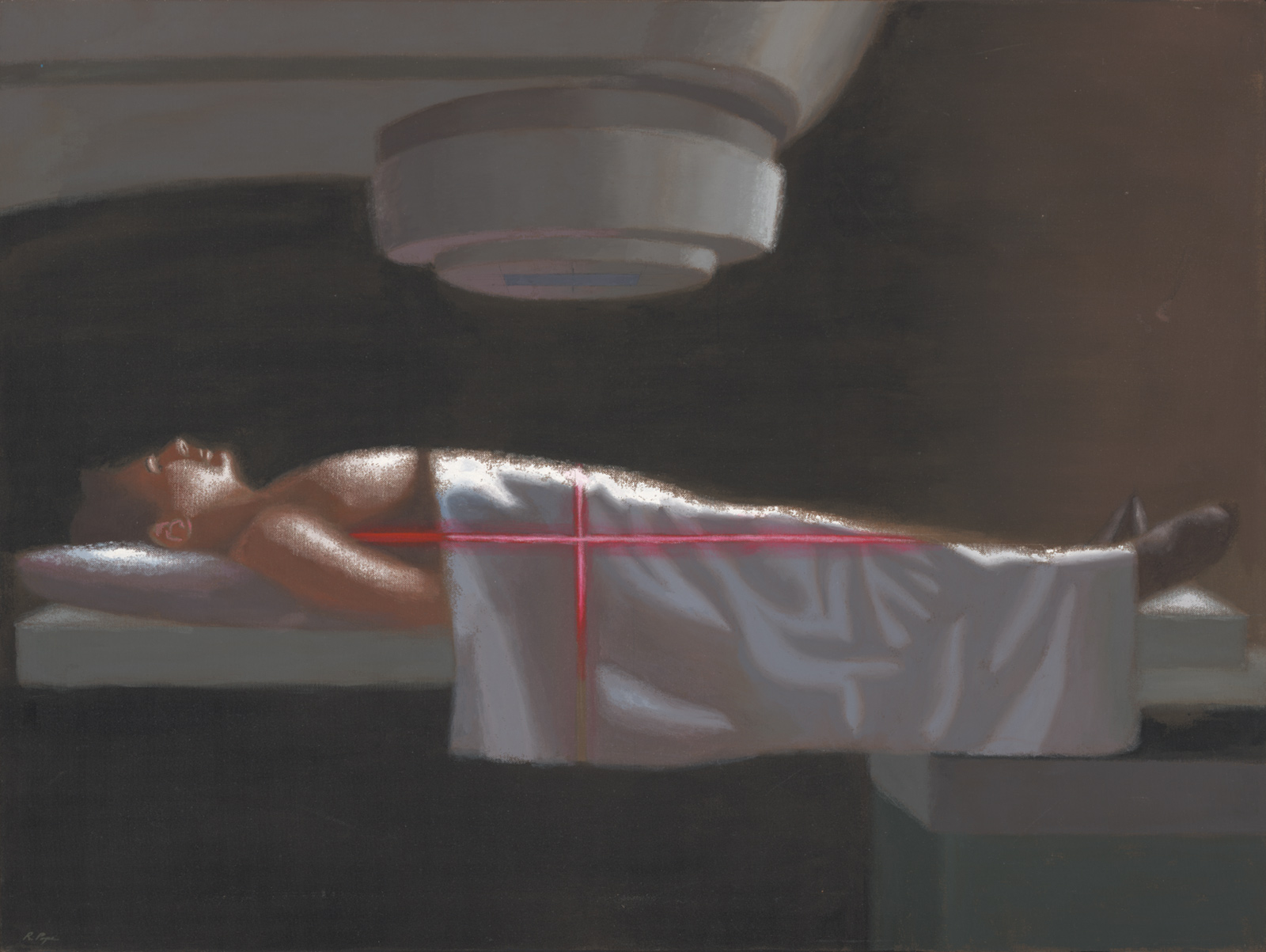
The loved one I lost was my mother. At the age of sixty-seven, she developed breast cancer. She openly told family and friends of her diagnosis, and what followed: surgery, to remove the breast mass and adjacent lymph nodes containing deposits of the tumor, and a combination of chemotherapy agents to reduce the risk of recurrence.
Several years later, the cancer returned. She knew then that the disease was incurable, but she also knew that there was hope to extend her life with treatment. “I am playing leapfrog with the cancer,” she told me. There were times when the chemotherapy took its toll, my mother too fatigued to do daily chores, attend synagogue, or see a movie or play. But there were also periods when life was lived fully.
Twelve years after the initial diagnosis, her oncologist, a thoughtful and dedicated doctor, told her that the cancer was growing quickly and treatment options were few. A drug had recently been approved by the FDA for pancreatic cancer. It was called gemcitabine, and there had been much controversy over its value. The clinical trials showed that the drug extended survival for several weeks, and critics decried the idea that a toxic drug with such minimal benefit would be brought to market. But soon after it became available, oncologists began studying its use in other cancers, including breast cancer, and there were some early encouraging data that it might be beneficial.
In addition, another way of targeting cancer, attempting to cut off its blood supply with a so-called anti-angiogenesis agent, Avastin, had been approved by the FDA. Although there was no formal protocol for doing so, her oncologist suggested combining gemcitabine with Avastin. There were real risks of toxicity, to be sure, and he was not pressing my mother to comply with his advice. But she very much wanted to live, and did not believe that the end was near. Remarkably, dual treatment resulted in fourteen months of remission, the cancer in her bones and liver shrinking markedly. She was able to visit me in Boston and go to concerts in New York, all the while taking the drugs.
Ultimately, the effects waned and the cancer grew explosively. Her oncologist said that she might enter so-called phase 1 studies, where new drugs are tested primarily to assess side effects with little expectation of benefit. She thought about it for a while, but concluded that the time had come. She arranged for hospice care at home and, mercifully, died in her own bed without pain or anxiety.
Dr. Vincent DeVita is an eminent oncologist whose work informs how I and many of my fellow cancer specialists approach the care of patients with lymphoma. He opens his memoir, The Death of Cancer, written with his daughter Elizabeth DeVita-Raeburn, with his family’s loss, that of a beloved aunt from cervical cancer. The narrative follows the arc of his efforts to combat cancer over the last fifty years, and asserts that we now have the tools—“skeptics be damned”—to eradicate it.
In 1963, DeVita, a newly graduated doctor, joined a group at the National Cancer Institute (NCI) that promoted chemotherapy for tumors when treatment of them primarily consisted of surgery and radiation. His mentors included Tom Frei and Jay Freireich, who combined single chemotherapeutic agents into the cocktail that first cured childhood leukemia. That success, DeVita argues, came from acting as transgressors, disregarding conventional boundaries in medical thinking.
DeVita, enthralled by the work of Frei and Freireich, wanted to repeat their success with leukemia. Along with several fellow trainees, including George Canellos, DeVita pursued Hodgkin’s disease, a deadly lymphoma. His group cobbled together four drugs, refining their doses and schedule of administration as they went along, rather than testing a set regimen. Then, when their series of doses was complete, they would analyze the data. The cure rate with the four-drug cocktail was so extraordinary that it was met with skepticism, if not downright dismissal, by many outside of the NCI.
DeVita recreates confrontations with critics at Memorial Sloan Kettering Cancer Center, which “had been built on land donated by the Rockefeller family; Laurance Rockefeller essentially owned the place”; its “clientele tended toward the rich and the international.” The Memorial doctors were using a version of his cocktail but had changed it to lower its doses. They were concerned about side effects of severe vomiting, nerve damage, and sepsis; and they failed to reproduce his stunning results. After a contentious session, DeVita concluded that the New York specialists had “made changes to satisfy their own egos.” Other oncologists who reduced the toxic doses
Advertisement
seemed less concerned about healing and more worried about being sued or maximizing their income. Patients couldn’t push for higher doses if they didn’t know that it mattered—and all a doctor had to do was omit that information.
Indeed, cancer patients should be fully informed of all potential risks and benefits, as my mother was.
Ultimately DeVita’s method of combining drugs at high doses, rather than backing away, proved to yield the greatest number of lymphoma cures. DeVita also was a fierce advocate of the work of Bernard Fisher, the pioneering surgeon at the University of Pittsburgh who showed that combining chemotherapy agents for women like my mother with cancer in the breast and adjoining lymph nodes delayed recurrence and, in some cases, resulted in long-term cures.
The flexible approach at the NCI, modifying a treatment in real time, is anathema to many clinical researchers. Constantly shifting variables, like dose and timing of drugs, makes it difficult to accurately assess either benefits or side effects. It also requires great trust in the probity of the clinicians conducting the trial—trust that they are able to make the right decisions as they alter the protocols as they go along. Traditionally, the FDA has rejected such an approach, requiring that a set protocol be carried through to its prescribed end. Yet some researchers are now harking back to DeVita’s strategy in what is called an “adaptive clinical trial,” by which statisticians work to devise novel methods, to distill meaningful conclusions about the outcomes. These methods include applying probabilistic assessments at prespecified times to allow changes in patient numbers, doses, and other parameters of the trial. (Recently, the FDA has stated it is open to considering adaptive trials in approving new drugs.)
In addition to adaptive clinical trials, DeVita believes in individual innovation; he writes that an oncologist should be free to draw on preliminary data and employ an agent not yet FDA-approved for a specific cancer. Gemcitabine, at the time approved only for pancreatic cancer, proved to be a highly effective and well-tolerated therapy for my mother’s breast cancer; how much added benefit, if any, she received from Avastin can be questioned, since this agent was ultimately ruled ineffective in subsequent clinical studies. Moreover, DeVita approaches treatment of each cancer patient with the mindset articulated by the great evolutionary biologist Stephen Jay Gould when he embarked on therapy for his own tumor. The median, he said, is not the message. The tail of the curve is worth aiming for, even in the most desperate cases.
Missing from DeVita’s glorification of mentors like Tom Frei is the history of treating breast cancer and other solid tumors with bone marrow transplant. Siddhartha Mukherjee, in The Emperor of All Maladies, his 2010 book on cancer, highlights Frei’s headstrong determination to administer high doses of toxic chemotherapy, even if the dose caused severe effects or brought the patient to the cusp of death. “If brute force was needed, then brute force would be summoned…. ‘We have a cure for breast cancer,’ Frei told one of his colleagues.” This galvanized a program at Boston’s Dana-Farber Cancer Institute, where Frei had moved after leaving the NCI. According to Mukherjee,
[the four-drug therapy for leukemia] had succeeded, Frei privately believed, not just because of the unique chemotherapeutic synergy among the drugs, but also because of the unique human synergy at the NCI—that cocktail of brilliant young minds and risk-taking bodies.1
But DeVita’s friend and peer George Canellos, who also moved to Dana-Farber, was deeply skeptical and vocally opposed Frei’s “cure.”
Over nearly ten years, some 40,000 women around the world underwent transplantation of bone marrow in order to cure breast cancer. Fortunately, my mother never did; her oncologist thought it not likely superior in benefit and could kill her. He and Canellos were right. Frei’s transplant program was an unmitigated disaster. There is an important lesson here for the reader that DeVita omits: inspirational figures can become wedded to a model that works in one type of cancer but is misconceived in another.
Working at the National Cancer Institute, within the Beltway, DeVita became adept not only in cancer medicine but in cancer politics. Biden’s “moonshot” metaphor echoed the language that President Nixon employed in asking Congress to declare a “war” on cancer in 1971.2 Nixon announced a timeline to win that war, five years, a gift for the bicentennial of 1976. Mary Lasker, a prominent Democratic Party contributor and philanthropist, and Benno Schmidt, a Republican who managed the Rockefeller fortune, together led the effort, and acted as DeVita’s political mentors.
Advertisement
DeVita offers an insider’s look at the manipulations and machinations that occurred, particularly the ways Lasker dealt with members of Congress to get her way. DeVita recalls accompanying Lasker to see Senator Hubert Humphrey:
We went right in, and they hugged and kissed and made small talk for about five minutes before Mary got around to introducing me. Before we went in, Mary had said to me, “I’m going to ask him for a $200 million increase over the president’s budget.” Panicked, I told her there was no way I could think of things to justify that kind of an increase. She gave me an angry look because she hated people to tell her they couldn’t spend money. She just told me to be enthusiastic and not to worry about it because she usually only got half of what she asked for anyhow.
DeVita acknowledges that the public was misled about the timeline of the war on cancer, but for what he believes was a greater good:
As we knew, the bicentennial celebration would come and go without a cure for cancer. And the predictable articles on the “failed” war on cancer started to appear in the mainstream press. “U.S. Cancer Program Termed ‘Sham,’” screamed a headline in March 1975 in The Boston Globe…. “War on Cancer Stirs a Political Backlash,” according to The New York Times in May 1975, while in the same year “False Front in War on Cancer” ran in the Chicago Tribune.
It misses the point to bristle at the media for holding the war’s proponents to their false promise. Just as a doctor should not lie to a patient, advocates for medical research should not lie to the nation to gain tax dollars.
In 1980, DeVita became the director of the NCI. Four years later, he provided Congress with a new goal in the war on cancer: a 50 percent reduction in cancer-related mortality by the year 2000. This did not occur, although the reduction was real: about 17 percent. In 2005, Andrew von Eschenbach, the subsequent NCI director, testified to Congress that he could “end all cancer suffering and deaths by 2015.” When Senator Arlen Specter, who had had cancer, pressed him about this assertion, von Eschenbach said that with more money he could do it by 2010.
In 1988, DeVita left the NCI to become physician-in-chief at Memorial Sloan Kettering Cancer Center. He lasted five years, clashing with Paul Marks, the president, who seemed to favor laboratory research over DeVita’s clinical programs:
Marks called a meeting…to announce my departure. I wasn’t there, but one of my former colleagues was. Later, he told me that Marks had said, “The problem with Vince is that he wants to cure cancer.”
DeVita, who then moved to Yale, confesses with a tone of embarrassment how he secured a large federal grant for its cancer center in the review process:
We played the game. We stretched the truth and told them that hallway conversations were formal program meetings, and the dean assured them that I was truly in charge. The president of the hospital promised continued unyielding support, which he never gave…. Twice, I got Yale’s core grant approved by finessing the truth.
Forty-five years after Nixon declared a war on cancer, success is most striking in our understanding of the biology of the disease. That biology is quite different from what was conceived by the experts around Lasker who were certain that viruses caused human tumors. Many millions of dollars were spent, and countless work hours expended, trying to find these putative human cancer viruses. The thinking was that when a single, common root for all cancers was identified, a single “silver bullet” would forever eradicate the disease.
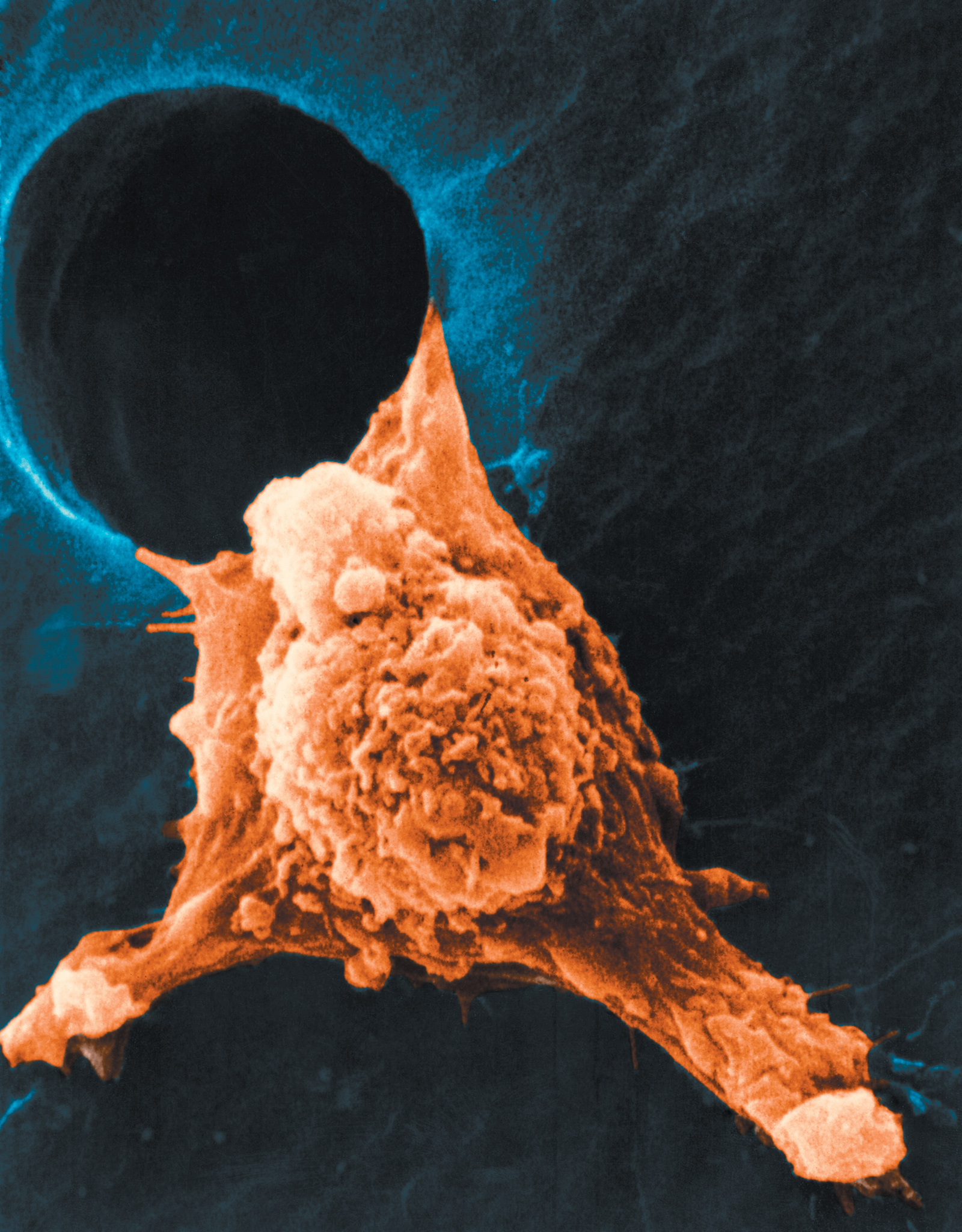
This proved not to be the case. Largely from the seminal work of Michael Bishop and Harold Varmus at the University of California, San Francisco, and Robert Weinberg at MIT, we discovered that cancer does not usually originate from the outside—through viruses—but we carry within ourselves the seeds of the malady, in the form of so-called oncogenes, i.e., genes that can be activated by chemical toxins, radiation, or random mutations. The proteins for which they code no longer control normal cell growth. There are also tumor suppressor genes that may act to counter the effects of oncogenes; when tumor suppressor genes are mutated, their restraining effects are lost. There is remarkable heterogeneity among cancers as both oncogenes and tumor suppressor genes mutate or amplify in number.
More daunting are recent studies showing that, within a single person, an initial cancer growing in an organ like the kidney can show a different array of mutations than the metastases emanating from it. As a result of these and a great many other developments, we now also recognize that “cancer” is a multiplicity of diseases; that even within the category of a single cancer type, like breast or lung, there are numerous subcategories. A tumor’s constant genetic changes may explain, in part, why so many treatments fall short; tumors have the nefarious capacity to alter their character and escape our grip, often likened to Proteus at the seashore.
Still, as DeVita rightly argues, we are now at a much better place than we were in past decades, not only in our biological knowledge but also in our treatment options, including success with immune therapies for, among others, melanoma and lung cancer. Such therapies, and there are now several of them, can stimulate the immune system to reject and destroy the growth of cancerous cells.
Recent statistics indicate a 23 percent drop in cancer deaths from 1991 to the present.3 Part of this decline is attributed to preventative strategies, like the campaign against smoking; part is due to early detection of otherwise lethal cancers, as with regular colonoscopies; and part from improved survival among patients with lymphoma, breast cancer, and other malignancies.
DeVita asserts that we could do much better; that if promising therapies were “used to their fullest potential…we could cure an additional 100,000 patients a year.” He does not show how he arrived at this number; physicians and scientists should have a basis for such claims, since such statistics tend to be repeated throughout American society.
DeVita puts part of the blame on the FDA. The agency is attacked from the right for being too slow in approving drugs and too concerned with side effects, and from the left as beholden to the pharmaceutical industry and far too ready to approve prematurely the release of drugs that turn out to have deleterious side effects. “Of course, both groups have taken things too far,” he writes. “Most of us recognize that we need regulations; we don’t want the FDA to go away. But we do want it to get out of the way.” Another obstacle is that
doctors risk FDA censure if they use an approved drug under any other circumstance, and patients are penalized because insurance companies won’t pay for treatments not approved by the FDA.
Most disturbing, some insurers now give doctors bonuses, up to $1,000 per patient a month, to prescribe the insurers’ protocols rather than decide autonomously what is best for a person.4
Dr. Richard Pazdur oversees review of oncology drugs at the FDA. DeVita casts him as an obstructionist. But recently Pazdur has modified his views on drug development, based in part on personal experience; his wife, an oncology nurse, developed metastatic ovarian cancer. Last November, the FDA approved more anticancer agents than at any time in the past.
Currently, there are more than seven hundred new cancer drugs and vaccines in development, the majority so-called “first in class,” representing approaches to treating cancer that are different from any other marketed therapy. These include nearly one hundred new agents for the treatment of lung cancer, eighty-seven for leukemia, seventy-eight for lymphoma, and seventy-three for breast cancer. The regulatory process at the FDA is accelerating, and some of DeVita’s concerns may become moot.5
In 2016, 1,685,210 new cancer cases and 595,690 cancer deaths are projected to occur in the United States. What will happen to these Americans is the principal concern of the new cancer initiative. But the false promises I have mentioned from Nixon, Lasker, and von Eschenbach also seem to be in the mind of Vice President Biden, who lost his son Beau last year to a brain tumor. Biden has become an active leader in the efforts against cancer. At the recent World Economic Forum, he said, “I’m not naive enough to think or suggest we are going to have a cure for every cancer…in the near term.” The NIH director, Francis Collins, a widely respected physician and scientist, embraced the initiative, but also sounded a note of caution: “We need to be careful not to overpromise, but…this is the moment to really pull out the stops.”6 To that end, the Obama administration will ask Congress for $1 billion to fund the initiative.
A “moonshot” to cure cancer boils down to an engineering problem. But there still are significant conceptual gaps in our knowledge, not merely technical ones. We have limited understanding about how cancers spread, the process of metastasis, and how tumors change to escape from the grip of targeted therapies directed against gene mutations.
In his recent appeals to doctors to make more progress on cancer, Vice President Biden concentrates on breaking down the “silos” in which he says information is held. He wants to encourage sharing of such information so that experts will be able to crunch “big data.” There are already big data undertakings, including CancerLinQ and GENIE. How much added value will come from combining databases in order to increase the information available is uncertain.
Biden also set a goal of making “a decade’s worth of advances in five years instead of ten, and eventually end cancer as we know it. We’re not looking for incremental changes, I’m looking for quantum leaps.” He did not define how advances per year will be measured, so that we know we’ve collapsed ten into five. In my view, a major impediment to a “quantum leap” is our inability to predict from laboratory studies which drugs will succeed in patients. Most agents we test fail in clinical trials, even though they target mutations and kill cancer cells in a petri dish or in animal models. Not only are we in need of new and more effective therapies, but we need a health care system that reliably delivers such therapies, particularly to underserved and poor populations.7 The high costs of new cancer drugs may make them beyond the reach of many people of limited means.
DeVita enumerates the many deficiencies that marked Nixon’s war on cancer, notably top-down management by self-serving bureaucrats, sweetheart contracts to friends, and costly clinical trials addressing trivial treatment issues. The progress over the past forty-five years in combating cancer arose largely from challenging authority and rejecting conventional thinking. That means skeptics in both science and policy should be eagerly welcomed, not damned.
-
1
Siddhartha Mukherjee, The Emperor of All Maladies (Scribner, 2010), p. 310. ↩
-
2
Jerome Groopman, “The Thirty Years’ War: Have We Been Fighting Cancer the Wrong Way?” The New Yorker, June 4, 2001. ↩
-
3
Rebecca L. Siegel et al., “Cancer Statistics, 2016,” CA: A Cancer Journal for Clinicians, Vol. 66, No. 1 (January/February 2016). ↩
-
4
Pamela Hartzband and Jerome Groopman, “How Medical Care Is Being Corrupted,” The New York Times, November 19, 2014. ↩
-
5
Jo Cavallo, “November Yields Record Number of FDA Approvals for New Oncology Drugs and Drug Indications,” The ASCO Post, December 10, 2015. ↩
-
6
Matthew Bin Han Ong, “Biden’s Cancer Moonshot to Focus on Bioinformatics and Data Sharing,” The Cancer Letter, January 22, 2016; and Matthew Bin Han Ong, “Obama Announces Moonshot to Cure Cancer,” The Cancer Letter, January 15, 2016. ↩
-
7
”Promising the Moon,” The Lancet, January 23, 2016. ↩