The National Institute on Drug Abuse estimates that 72,000 Americans died from drug overdoses in 2017, up from some 64,000 the previous year and 52,000 the year before that—a staggering increase with no end in sight. Most involved opioids.
A few definitions are in order. The term opioid is now used to include opiates, which are derivatives of the opium poppy, and opioids, which originally referred only to synthesized drugs that act in the same way as opiates do. Opium, the sap from the poppy, has been used throughout the world for thousands of years to treat pain and shortness of breath, suppress cough and diarrhea, and, maybe most often, simply for its tranquilizing effect. The active constituent of opium, morphine, was not identified until 1806. Soon a variety of morphine tinctures became readily available without any social opprobrium, used, in some accounts, to combat the travails and boredom of Victorian women. (Thomas Jefferson was also an enthusiast of laudanum, one of the morphine tinctures.) Heroin, a stronger opiate made from morphine, entered the market later in the nineteenth century. It wasn’t until the twentieth century that synthetic or partially synthetic opioids, including fentanyl, methadone, oxycodone (Percocet), hydrocodone (Vicodin), and hydromorphone (Dilaudid), were developed.
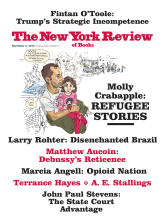
In 1996 a new form of oxycodone called OxyContin came on the market, and three recent books—Beth Macy’s Dopesick, Chris McGreal’s American Overdose, and Barry Meier’s Pain Killer—blame the opioid epidemic almost entirely on its maker, Purdue Pharma. OxyContin is formulated to be released more slowly and therefore lasts longer. The company claimed that the drug’s slow release would make it less addictive than ordinary oxycodone, since the initial euphoria—the high—would be muted. Based on this theory and little else, the FDA permitted OxyContin to contain twice the usual dose of oxycodone and carry on the label this statement: “Delayed absorption, as provided by OxyContin tablets, is believed to reduce the abuse liability of a drug.” (The FDA official who oversaw OxyContin’s approval later got a plum job at Purdue Pharma.)
The company launched an extraordinarily aggressive and successful marketing campaign to convince physicians that they had the holy grail of a nonaddictive opioid. It sent hundreds of sales representatives to doctors’ offices to tout OxyContin, and offered doctors dinners and trips to meetings at luxury resorts. And it paid more than five thousand doctors, pharmacists, and nurses to train as speakers to tour the country promoting OxyContin. But like all opioids, OxyContin is addictive. And soon enough, users found that they could crush the pills or dissolve the coating, then snort the drug like cocaine or inject it like heroin. Each pill would then become essentially an instantaneous double dose of oxycodone.
OxyContin almost immediately became a blockbuster—that is, a prescription drug with annual sales of more than $1 billion. It was widely used not just by those for whom the prescriptions were written, but by their relatives and friends. The pills were also sold or stolen or otherwise diverted to street use. In addition, “pill mills” sprang up, where unethical physicians wrote innumerable prescriptions for OxyContin and refilled them automatically without ever seeing the patient. McGreal describes “one of the most productive pill mills in the country,” which operated in the small town of Williamson, West Virginia—known locally as “Pilliamson.” The town, he says, “was awash in pills,” and people came by car and bus to line up at the clinic and cooperating drugstores. “Investigators calculated that in 2009 alone, the clinic pulled in $4.6 million in a town with a population of little more than three thousand people.”
It’s impossible to know how many new prescriptions were obtained in each of these ways, but one way or another, OxyContin addiction grew into an epidemic. The epicenter was central Appalachia, and its victims were mainly white people in small, economically depressed coal-mining communities in southern West Virginia and parts of Kentucky, Tennessee, and southwestern Virginia.1
The three books that focus on Purdue Pharma are in a sense the same book. Barry Meier first published Pain Killer in 2003. The new edition (released by a different publisher) is much the same, with some updating and re-arrangements. The two new books, Dopesick and American Overdose, cover the same story as it unfolded in the same region of the country. Both Macy and McGreal refer to the 2003 edition of Meier’s book (but not the new edition, probably because they could not have known of it at the time their books were written). All three books are gripping and well written, with detailed accounts, one after another (perhaps too many), of families decimated by the epidemic. And they all tell the story of Art Van Zee, a physician in southwestern Virginia, who in 2000 became aware of the growing epidemic of OxyContin there and tried heroically to get Purdue Pharma and the FDA to take responsibility for it.
Advertisement
Purdue Pharma and the Sackler family that founded it are very hard to defend. By aggressively marketing OxyContin, even after they knew it was being widely abused, the family became enormously wealthy. But the FDA was also guilty. It permitted OxyContin to be sold as a relatively nonaddictive opioid without good evidence to support that claim, and it should have been obvious that the pills might be crushed or dissolved to make them even more addictive. Van Zee, along with Beth Davies, a nun who ran the local substance abuse clinic, saw Lee County, Virginia, blanketed with OxyContin prescriptions and watched the deaths mount, particularly among young people. They informed Purdue, which simply stonewalled. Over the following year, Van Zee devoted himself completely to the cause, meeting with company and FDA officials and testifying before a Senate committee, trying to get Purdue to reformulate the drug or even withdraw it from the market.
In 2007 Purdue pled guilty to criminal charges of fraudulently marketing OxyContin and settled for $600 million in fines and penalties. Three executives pled guilty to misdemeanor charges and were sentenced to four hundred hours of community service and lesser fines. The company’s fine was trivial in comparison with its profits from OxyContin. In fact, almost every other major pharmaceutical company has had to settle both civil and criminal charges of fraudulent marketing for much more (the record settlement is now GlaxoSmithKline’s $3 billion, for a variety of violations, including falsely promoting drugs and failing to report safety data). These kinds of fines are just the cost of doing business. And so it was for Purdue Pharma, although the fraudulent marketing stopped and a warning was added to the label.
The problem with these three books, and it’s a big one, is that they treat the Purdue story as though it were the whole story of the opioid epidemic. But OxyContin did not give rise to opioid addiction, although it jump-started the current epidemic. Heroin has been a common street drug ever since it was banned in 1924. Morphine has also been widely abused.
Nor would taking OxyContin off the market end the epidemic. The overwhelming majority of opioid deaths are caused not by OxyContin but by combinations of fentanyl, heroin, and cocaine, often brought in from China via Mexican cartels, and frequently taken along with benzodiazepines (such as Valium or Xanax) and alcohol. These drugs are cheaper and stronger, particularly fentanyl. Fentanyl was first synthesized in 1960, and soon became widely used as an anesthetic and powerful painkiller. It is legally manufactured and highly effective when used appropriately, often for short medical procedures such as colonoscopies. The illicit production and street use is relatively new, but it is now the main cause of most opioid-related deaths (nearly 90 percent in Massachusetts).
The steady increase in opioid deaths after OxyContin came on the market has been supplanted by a much faster increase starting around 2013, when heroin and fentanyl use increased dramatically. We now have two epidemics—the overuse of prescription drugs and the much more deadly and now largely unrelated epidemic of street drugs. By concentrating on the first, we are closing the barn door after the horse is long gone.
Efforts to deal with the epidemic have been all over the map—literally. Possession of illegal drugs (and legal drugs illicitly used) is still a federal crime, and prisons are still full of people whose only crime was that. But many states, counties, and cities have begun to regard opioid addiction as a public health issue, not a police issue. They are opening centers in which people who seek help are shifted to less powerful opioids like methadone and buprenorphine (Subutex)—a method known as “medication-assisted treatment,” or MAT. Naloxone (Narcan), the antidote for an opioid overdose, is now sold over the counter in almost all states. If used immediately, it can prevent an otherwise inevitable death from a drug overdose. And drug courts, which may drop criminal charges in return for an agreement to submit to treatment and monitoring, are becoming more common.
Most controversial are facilities called “safe injection sites,” or SIFs, where drug users can come to use drugs without fear of arrest. The staff provides clean needles to reduce the risk of HIV and hepatitis C infections, and is prepared to resuscitate addicts who overdose. This approach is called “harm reduction.” The problem is that addicts must still buy drugs illegally, and it’s almost impossible to know exactly what is in them.
In a recent New York Times Op-Ed, the deputy attorney general, Rod Rosenstein, came down hard on SIFs. He warned that “it is a federal felony to maintain any location for the purpose of facilitating illicit drug use,” and that “cities and counties should expect the Department of Justice to meet the opening of any injection site with swift and aggressive action.” He was referring to plans to operate SIFs in San Francisco, New York City, and Seattle, and similar options now being considered by Colorado, Maine, Massachusetts, and Vermont. Later in the same article, however, he softened, saying we should “help drug users get treatment and aggressively prosecute criminals who supply the deadly poison,” suggesting that perhaps he doesn’t believe simple possession is so bad, after all.
Advertisement
But the proposed solutions to this epidemic range from the extreme of “lock ’em up” to “drug abuse is no less a disease than cancer or diabetes” and should therefore be met with the same solicitude. Ryan Hampton exemplifies the latter view in his angry book, American Fix. A former drug user himself and now an impassioned advocate and activist, he insists that drug abuse should be regarded like other diseases. He doesn’t acknowledge that for most users there was a moment of choice in becoming addicted that is not the case for people with cancer or diabetes. After receiving Dilaudid for a painful ankle, Hampton decided to ask for more, and then more. I think one can make the argument for sympathy with drug users and for understanding how the quest for drugs ceases to be under their control without claiming an analogy to diseases like cancer or diabetes.
Hampton paints a vivid picture of the downward spiral of addiction. When he “leveled up to IV heroin,” he explains, “it was cheaper than pills, easier to get hold of, and a quarter the cost. More important, nobody was tracking us in a database.”
Where Hampton is at his best is in his exposure of the profiteering and corruption in the burgeoning addiction industry—what he calls “the treatment industry swamp.” In the swamp, he found
lack of effective treatment, exorbitant costs, and ridiculous twenty-eight-day vacations disguised as medical help, fed by patient brokers who run a completely legal, high-end human trafficking cartel to push tens of thousands of patients through the broken system.
He was referring to the panoply of treatment centers, both residential and outpatient, and detox facilities, where users are supposed to be weaned from drugs before entering “sober living houses.” As in so much of American medicine, even nonprofit insurers like Medicaid outsource the actual delivery of care to for-profit companies that charge whatever the market will bear. According to Hampton, “one of the most expensive treatment centers in America, Passages Malibu, costs more than $60,000 per month.” Costs are settled by a crazy quilt of payers, including state and local governments, Medicaid, other federal programs, private insurers, and often by desperate families. Not surprisingly, only a minority of users are ever treated.
In 2017 the Aspen Institute’s Health Strategy Group, led by two former secretaries of health and human services, Tommy Thompson and Kathleen Sebelius, and consisting of twenty-four members from various health-related fields (I am among them), met for three days to examine the opioid epidemic. The deliberations were preceded by four presentations by experts in the field. In the final broad and comprehensive report, the group made a strong case for decriminalizing drug addiction and instead regarding it as a public health issue. Among the five major recommendations was a call for more research into nearly all aspects of the epidemic. It’s startling how little we know, given the immensity of the problem and the media attention it receives.2
We need to know, for instance, how effective opioids are for different kinds of pain, including long-term treatment for chronic pain. We need to know how opioids compare in effectiveness and side effects with acetaminophen (which can cause liver failure) and nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (which can cause gastrointestinal bleeding). We need to know how the death rate in the opioid epidemic compares with the rate of use. We know the death rate is soaring, but does that mean the rate of use is, too, or is it simply a result of the lethality of the drug mixtures obtained on the street? We need to know how much diversion there is now from legitimate treatment to abuse. That includes diversion of methadone and buprenorphine, which are also opioids and can be sold on the street or added to the user’s illicit intake. According to Macy, “Buprenorphine is the third-most-diverted opioid in the country, after oxycodone and hydrocodone.”
We need to know how many addicts want to quit, since most don’t seek treatment. Why don’t they? And finally, we need to know the best approach to treatment. There is concern, for example, that detox might be dangerous, because the first dose after a relapse can be deadly if the user is no longer tolerant to the drug’s effects. Is providing methadone or buprenorphine indefinitely, even for life, the best treatment among bad choices? There is plenty of speculation about all of these questions, and suggestive findings about some of them, but little solid evidence.
We also need to remember an essential and crucial fact: opioids do have a legitimate purpose, and it’s an enormously important one. They treat severe pain, often when no other treatment is effective. Patients suffering from cancer are sometimes completely dependent on opioids for relief, as are some patients with other forms of severe pain. As the authors of the books acknowledge, pain was systematically undertreated throughout most of the twentieth century. After centuries of free and easy use of opioids, there was a sudden reaction in the United States at the start of the twentieth century, which had much to do with anti-immigrant sentiment, particularly animus toward Chinese immigrants who were widely assumed to be opium addicts. (It also paralleled the growing reaction against alcohol that resulted in Prohibition.) The 1914 Harrison Narcotics Tax Act imposed strict regulations on the use of opioids; they had to be prescribed by physicians, and then only for patients not already taking them. Prohibition lasted for only thirteen years, but the dread of opioid addiction stayed with us until the 1980s and caused cruel suffering for generations of patients.
Even in hospitals where cancer patients lay dying in agony, opioids were administered reluctantly, in small doses, and at infrequent intervals. When I was in training in a teaching hospital in the 1960s, there was an awful ritual to it. The drugs were administered according to a pro re nata (prn) regimen (ostensibly “as needed”) that required the patient to wait out a four-hour interval, no matter how severe the pain, and then request the next dose. Those who badly wanted the drug had to keep track of the time and have the strength and endurance to summon a nurse if one was nearby. Patients were sometimes inhibited in asking for the next dose by a desire to please the medical staff and not be a nuisance, or by their own belief that taking morphine was somehow wrong or reflected weakness. The extent to which nurses and physicians shared the common fears of addiction influenced their readiness to respond. Desperate patients would count the minutes toward the end of the interval, hoping they could flag down a nurse. Many doctors and nurses interpreted the anxiety and clock-watching as a sign of growing addiction, not inadequate pain relief. These patients were labeled “drug-seeking” and often punished for it by being denied the very help they needed.
During the 1980s there was a welcome change in that attitude, partly due to the hospice movement that had begun in the United Kingdom. The prn system became more flexible, or was eliminated altogether. There was a realization that because pain is entirely subjective, there is no way to measure or verify it, and even patients with the same condition could differ in their experience of pain. Instead of having to flag down nurses, patients were asked at shorter intervals whether they needed pain relief, and how much. In 2001 the Joint Commission on the Accreditation of Healthcare Organizations proclaimed pain the fifth vital sign, to be assessed in every patient, along with heart rate, respiratory rate, temperature, and blood pressure. Although the motivation for this move was laudable, it presented problems, since, unlike the other four vital signs, pain can’t be objectively quantified.
The authors of the books under review recognize the history of inadequate treatment of pain throughout most of the twentieth century, but they don’t give it its due. They concentrate instead on the reaction of the 1980s, which they consider excessive and an underlying cause of the opioid epidemic. In 1982 I wrote an editorial in The New England Journal of Medicine, which began, “Few things a doctor does are more important than relieving pain.” I still believe that. I ended with these words: “Pain is soul-destroying. No patients should have to endure intense pain unnecessarily. The quality of mercy is essential to the practice of medicine; here, of all places, it should not be strained.”
The opioid epidemic, while horrifying, is still outweighed by alcohol deaths, which are also increasing, according to the Centers for Disease Control. Hampton writes, “If my first drug of choice came with a prescription, the second one, alcohol, was culturally embedded and used to celebrate at every turn of events.” In 2016, when there were 64,000 deaths in the US from the drug epidemic, there were 90,000 from alcohol (including accidents and homicides caused by inebriated people, as well as direct effects, mainly cirrhosis of the liver). Cigarette smoking is estimated to cause 480,000 deaths a year. I do not intend to minimize the opioid epidemic. Far from it. What I want to underscore is the differences in these three epidemics. Alcohol and cigarettes have no medical or practical uses of any kind. Yet we permit their use if regulated. In contrast, opioids do have medical uses, and they are important.
The opioid epidemic is usually seen as a supply problem. If we can interdict the supply of prescription opioids, the thinking goes, we can stanch the epidemic. But that is unlikely to work for two reasons. First, as I pointed out, this is no longer mainly an epidemic of prescription drugs but of street drugs. And second, it creates an onerous obstacle for doctors and outpatients who require pain treatment. More and more, they have to satisfy regulations expressly designed to restrict access to prescription opioids. Some make sense. For example, it’s reasonable to monitor opioid prescriptions to detect pill mills. It’s also reasonable to flag users who “doctor-shop,” that is, see several doctors at once to try to get multiple doses of opioids.
But other requirements are meant simply to inconvenience both doctors and patients until they give up. For example, in Massachusetts doctors must limit their first-time opioid prescriptions to seven days. That can be more than an inconvenience for ill patients in pain. Macy quotes a letter from a friend with severe back pain from scoliosis. “‘My life is not less important than that of an addict,’ my friend wrote,…explaining that her new practitioner requires her to submit to pill counts, lower-dose prescriptions, and more frequent visits for refills, which increase her out-of-pocket expense.” Even more serious is a new shortage of opioids for injection in cancer centers.
For physicians, who are already weighed down by innumerable bureaucratic requirements, these restrictions present one more hoop to jump through, and many simply won’t do it. Instead, they’ll send the patient away with some Advil and hope it does the trick, even though they know it probably won’t. The regulations are having their intended effect. In Massachusetts, opioid prescribing has decreased by 30 percent. Meanwhile, the epidemic of street drugs continues apace. McGreal raises the possibility that reducing access to prescription opioids might feed the demand for heroin. Macy quotes an addiction specialist who laments that “our wacky culture can’t seem to do anything in a nuanced way.”
I believe the modern opioid epidemic is now more a demand problem than a supply problem. Three years ago, the Princeton economists Anne Case and Angus Deaton published an explosive paper about the surprising rise in mortality, starting at the turn of this century, among middle-aged white non-Hispanic men and women. The increase was greater in women than in men. They found three main causes: drug and alcohol overdoses, suicide, and alcohol-associated liver disease. They later called these “deaths of despair,” because they were most common among workers in tenuous jobs, with only a high school education or less, who were struggling to stay afloat in isolated regions of the country. Dragged down by these deaths, in the past three years overall life expectancy in the United States has started to drop.
It’s not hard to see reasons for the despair. Most working-class Americans have not benefited from our booming economy, the fruits of which have gone almost entirely to the richest 10 percent. For the bottom half of the population, income has scarcely budged since the 1970s, while expenses for necessities like housing, health care, education, and child care have skyrocketed. In Appalachia, where the opioid epidemic first took hold, many coal miners were unemployed and would probably remain so. People expected they wouldn’t live as well as their parents had, and had little hope for their children. It is true that African-Americans still have higher overall mortality rates than whites, but that gap is closing rapidly for people under the age of sixty-five, particularly for women. By 2027, white women will have higher mortality rates than African-American women. Mortality for African-American men is falling even faster than for African-American women; it is projected to be equal to that of white men by 2030. But the epidemic has extended to all parts of the country and to all ethnic groups, so it’s unclear how the effects will be distributed in the future.
By the middle of this decade, the grotesque inequality in this country began to get the attention it deserves. And the growing awareness of that inequality fed the populist passion that, when twisted and distorted, produced the election of Donald J. Trump. It’s probably not coincidental, then, that the opioid epidemic got its second wind at about that time. It certainly marks the time when the opioids of choice changed from prescription drugs to the witches’ brew of street drugs. Did the epidemic explode because people were becoming aware that the American Dream was no longer theirs to dream?
As long as this country tolerates the chasm between the rich and the poor, and fails even to pretend to provide for the most basic needs of our citizens, such as health care, education, and child care, some people will want to use drugs to escape. This increasingly seems to me not a legal or medical problem, nor even a public health problem. It’s a political problem. We need a government dedicated to policies that will narrow the gap between the rich and the poor and ensure basic services for everyone. To end the epidemic of deaths of despair, we need to target the sources of the despair.
This Issue
December 6, 2018
Saboteur in Chief
That Formal Feeling
-
1
The books by Macy and McGreal provide full accounts of the development and promotion of OxyContin, the onset of the epidemic in Appalachia, the failure of Purdue to respond, and the company’s eventual admission to fraudulent marketing. ↩
-
2
This report is available at www.aspeninstitute.org/publications/confronting-our-nations-opioid-crisis. ↩